Foreword
Douglas E. Schmidt, a personal injury lawyer with over 40 years experience in handling neck and back injuries resulting from CAD (Cervical Acceleration/Deceleration) trauma says this:
DMX is the single greatest medical development in my 40 year career as a personal injury lawyer. Combined with CRMA analysis and multi-positional upright MRIs, we now have solid objective proof of ligamentous and disc injuries that couldn’t be objectively proved in the past.
We have known for many years that ligamentous injury is at the core of all Cervical Acceleration/Deceleration injuries (CAD). However, until recently there was no objective proof of ligamentous injuries. DMX now provides that proof.
For the first part of my legal career as a personalinjury lawyer, we didn’t have MRIs—and, in turn, no imaginable proof of disc injuries. When I started seeing MRI scans proving the existence of disc injuries, I was sad for all of those past clients who didn’t get justice because they couldn’t prove their disc injury.
I am now seeing case after case where my clients’
ligamentous injuries are now objectively proven. I can’t help but reflect on all the victims of whiplash injuries that haven’t received the justice they deserved because there was no objective proof of ligamentous injuries.
Now, the good news!!! This combination of technology has come together as the biggest single medical advancement of my 40+ year legal career!!!
The Golden Triangle now provides objective proof of ligamentous injury and the devastating consequences of the accelerated degeneration that follows:
-Digital Motion X-ray (DMX);
-Computerized Radiographic Mensuration Analysis (CRMA);
-Motion MRI.
Virtually 100% of the DMX’s that have been done on my clients have revealed objective proof of ligamentous laxity. (They have been carefully selected, i.e. the majority being clients with significant symptoms lasting more than 1 year after the car accident.)
It is well established in the medical literature that flexion extension trauma results in accelerated degeneration of the spine including the intervertebral discs. Until recently, that has only been a theoretical concept based on clinical observations. Recently, I have “circled” back and sent a number of my client back for repeat MRIs. The results have been astounding, showing clear proof of shockingly accelerated degeneration of the intervertebral discs in a matter of just a few years. See Appendixes A and B for case examples.
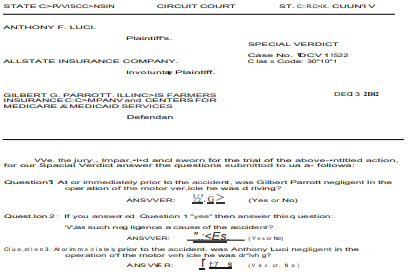
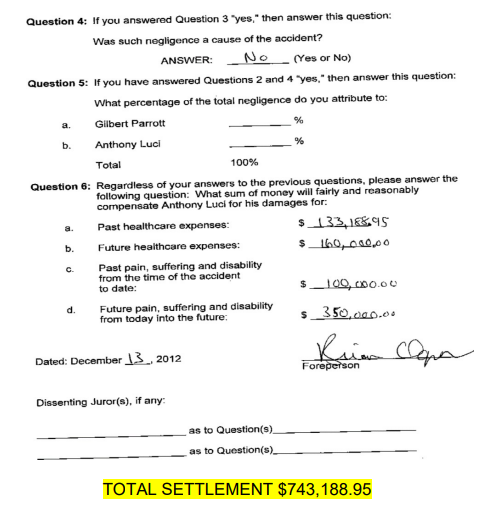
The evidence that DMX videos provides in the court room setting is also amazing. In the very first case in which DMX was introduced as evidence in a court trial, the jury was obviously fascinated. They “scooched” forward on their seat, craned their necks forward, and stared “buggy-eyed” at the screen as the DMX film played out. The result was a jury verdict of $743,188.95 in a case where the last formal offer before trial was only $10,000.00. See Appendix C for a copy of the jury verdict in that case.
DMX is an amazing technological development. It is well recognized and respected in the medical literature—but the large majority of the medical community has virtually no knowledge of it. It has been accepted as reliable evidence in court in a number of cases. The courts and arbitrators have accepted DMX/CRMA in nearly 50 cases where the Schmidt Law Firm has represented the injury victim without a single case where it has been rejected.
The purpose of this Handbook is to provide basic information about the value of DMX in medical, chiropractic and legal practice.
Respectfully submitted,
Douglas E. Schmidt
Schmidt Law Firm
952-473-4530
schmidtlaw@visi.com
TABLE OF CONTENTS
DMX Provides Objective Proof for the Diagnosis of Ligamentous Injuries
- Ligamentous injury is at the core of all CAD (Cervical Acceleration/ Deceleration) injuries.
- CAD trauma causes stretching of cervical ligaments beyond their anatomical limit.
- Over-stretching of ligaments causes “plastic” deformity.
- Many injuries of the cervical spine are ligamentous injuries which are permanent.
- “Sub-failure” (stretch only- no tear) ligamentous injuries are serious!
- Ligamentous Damage causes Instability of the Spine.
- Ligament injuries produce two types of “motion segment” impairment- translational and angular.
- It’s all about motion!!!
- How does DMX work?
- DMX can detect ligamentous laxity that static X-rays cannot see.
- DMX is respected by the chiropractic community.
- DMX is respected by the U.S. Government.
- DMX is respected by the medical community.
- DMX has been accepted as reliable evidence by the courts.
- CRMA can quantitatively analyze the extent of the ligamentous laxity.
- CRMA can be used to establish a percentage of impairment rating using the AMA Guides rating system.
- DMX scans can be used to provide an AMA-based disability rating.
- How we know that the ligamentous laxity was caused by CAD trauma.
- Ligamentous laxity causes accelerated degeneration of the intervertebral discs.
- When ligamentous laxity is demonstrated, later repeat MRIs can, in some cases, objectively prove accelerated degeneration.
- DMX, and Weight-Bearing MRI can be extremely valuable in proving major impairment hat previously were dismissed as minor “soft tissue” injuries.
- Flexion-Extension MRIs provide a method for detecting herniationsthat are not observable in conventional MRIs.
- DMX provides proof of the cause of Facet Joint Injuries.
- Ligamentous laxity is the primary cause of Myofascial Pain Syndrome and trigger points.
- Case studies-“Gina’s Case” and “Bruce’s Case”, provide objective proof of accelerated degeneration of intervertebral discs secondary to ligament damage.
- The most important aspect of facet joint injuries is being overlooked in many cases, namely the ligamentousinjury.
Appendix A- Records from “Gina’s Case”
Appendix B- Records from “Bruce’s Case”
Appendix C- “Tony’s Case”-The jury verdict of $743,188.95
Ligamentous injury is at the core of all CAD (Cervical Acceleration/Deceleration) injuries.
It is well known that ligament damage is at the core of all Cervical Acceleration/Deceleration injuries (CAD also known as flexion/extension injuries or “whiplash” injuries.)
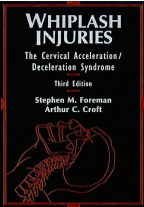
Foreman/Croft in their classic textbook, Whiplash Injuries: The Cervical Acceleration/Deceleration Syndrome explains this basic concept:
Ligaments and related structures such as the fascia and the discs are also damaged or disrupted in CAD trauma. Both the ALL
(Anterior Longitudinal Ligament) and the posterior ligamentous complex (intervertebral disc, zygapophyseal joint
capsules, posterior longitudinal ligament, ligamentous flavum, interspinous ligament, and the ligamentum nuchae)
have been shown experimentally…to rupture, either partially or completely. Ligaments of the upper cervical spine,
such as a cruciform ligament, the suspensory and apical ligaments of the dens, and the alar ligaments also have
been found to be ruptured or disrupted.
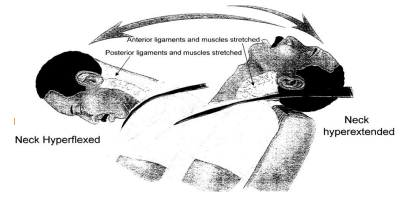
CAD trauma causes stretching of cervical ligaments beyond their anatomical limit.
CAD forces cause hyperextension and hyperflexion of the cervical spine.
Hyperextension has been proven to cause damage to the anterior longitudinal ligament (ALL) and the facet capsular ligaments. Studies have proven that 50-60% of the victims of chronic pain lasting more than one year post accident have facet joint injury as the primary source of their pain. See Lord et. al., “Chronic cervical zygapophysial joint pain after whiplash: a placebo-controlled prevalence study,” which was published in Spine 1996; 21(15):1737-1745.
Recent research reported in the Journal of Biomechanics reported that injury to the apical and alar ligaments is common as the result of CAD trauma, with damage to the alar ligaments occurring in 66% of whiplash victims. See Fice et.al. “Investigation of whiplash injuries in the upper cervical spine using the neck model,” Journal of Biomechanics, 45(6), 1098-1102 (2012).
Hyperflexion has been proven to cause damage to the ligamentous flavum and the interspinous ligaments.
Over-stretching of ligaments causes “plastic” deformity.
Over-stretching, or excessive distension (hyper-elongation), of the cervical ligaments results in “plastic” deformity instead of “elastic” deformity.
“Elastic” deformity is that which returns to its original shape, like a rubber band.
“Plastic” deformity is that which does not return to its original state and, thus, results in the ligament remaining “stretched.” In other words, once stretched, always stretched.
A frequently used analogy is that of the plastic holder for a six-pack of soda pop. When one pulls a can out of the plastic holder, it stretchesout of shape and does not return to its original shape. The plastic holder will no longer hold the can if one attempts to put it back. That is exactly what happens with an over-stretched ligamentous injury.
Many injuries of the cervical spine are ligamentous injuries which are permanent.
Plastic deformation is, by definition, permanent. Overstretched ligaments heal with scar tissue. The following photographs show the abnormal scar tissue formation in ligaments that have been injured due to abnormal stretching in flexion-extension injury.
As stated in Foreman/Croft, “The healing of ligamentous structure is generally incomplete” (p. 183) and “plastic deformation or ligamentous ‘sub failure’ (which is) still present after 4 months is likely to be permanent.” (p. 185)
“Sub-failure” (stretch only-no tear) Ligamentous Injuries Are Serious!
Ligamentous injuries are classified in the medical literature in two categories:
- Failure Injuries-involving a total tear orrupture;
And
- Sub-failure Injuries involving a “stretching” without tear or rupture.
Recent studies have proven that “sub failure” ligamentous injuries can be as serious and often more serious than “failure” ligamentous injuries! A recent article which appeared in the Journal of Biomechanics reported studies done at the Orthopedic Bioengineering Research Laboratory of Colorado State University where they took anterior longitudinal ligaments (ALL) and ligamentum flavum (LF) from cadavers and subjected them to whiplash-type trauma. The results were:
- Stretch (distension) damage resulted in abnormal laxity equal to having “no ligamentous support” at all!!!
- Partial injury to these ligaments resulted in laxity equivalentto “completely compromised” ligaments.
Leahy, et al., “The Effects of Ligamentous Injury in the Lower Cervical Spine,” Journal of Biomechanics, 15:2668-2672 (2012).
Ligamentous damage causes instability of the spine.
Instability of both the cervical and lumbar spine from trauma or the resulting degeneration is recognized as a significant contributor to neck and lower back pain and disability. Lin, “Characteristics of Sagittal Vertebral Alignment in Flexion Determined by Dynamic Radiographs of the Cervical Spine,” Spine, Vol. 26, No 3, pp 256-261 (2001).
The American Academy of Orthopedic Surgeons defines instability as “Segmental instability (which) is an abnormal response to applied loads, characterized by motion in motion segments beyond normal constraint.” See American Academy of Orthopedic Surgeons, A Glossary on Spinal Terminology, 1985:34.
Ligament injuries produce two types of “motion segment” impairment
translational and angular.
The primary function of ligaments is to hold the vertebrae inplace. Ligamentous “stretch” injuries produce ligamentous laxity. Ligamentous laxity, in turn, causes abnormal movement of the vertebrae that can be seen on X-ray. The ligaments don’t show up on the DMX. However, the abnormal positioning of the vertebra in the cervical spine does show upon an X-ray. It is a simple fact that the function of ligaments is to keep the vertebrae in their normal anatomical position. Abnormal positioning of the vertebrae results from ligamentous laxity. Therefore, the abnormal positioning of the vertebrae proves the damage of the ligaments, i.e. ligamentous laxity.
Medical literature has long ago established two types of motion segment impairment resulting from ligamentous laxity:
- Translational irregularity and 2. Angular irregularity.
The AMA Guides has, since 1993 recognized the concept of “Alteration of Motion Segment Impairment” (AOMSI). The AMA Guides to the Evaluation of Permanent Impairment, 4th Ed (1993) illustrated the concepts of Loss of Motion Segment Integrity, both in terms of “translation” motion and angular motion as follows:
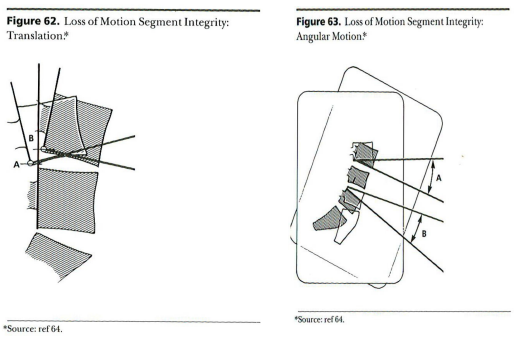
Foreman/Croft are in total agreement. They used a similar illustration of the same concept in 1995:
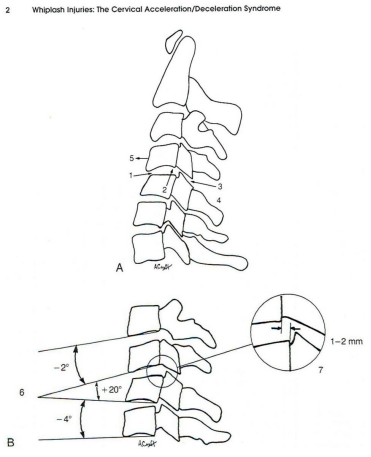
Loss of translational motion segment integrity can result in both retrolisthesis (the backward displacement of one vertebra in relation to the vertebral body immediately below it) or anterolisthesis (forward displacement). Trauma is a well-recognized cause.
See the illustration below which shows both anterolisthesis (top left) and retrolisthesis (bottom left) due to rupture of the capsular ligament:
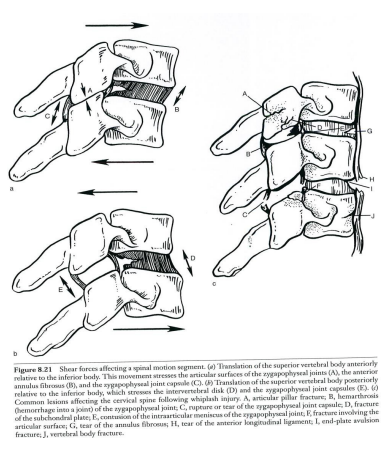
Note: Medical research has proven that overstretching of these ligaments without tear or rupture results in almost the same amount of laxity aswith a tear or rupture.
It’s all about motion!!!
Most patients complain that their worst pain is with movement, and repetitive movements that aggravate their symptoms, producing muscle spasm, myofascial pain, and disability. It is motion that causes the symptoms. It makes perfect sense that scanning during motion is more likely to reveal the problem.
In simple language, when people
are hurt in motion, diagnostic tests
must be done in motion to properly
detect the full extent of
the problem. DMX does that!!!
As the old saying goes, “The proof is in the pudding.” Anyone who has actually watched DMX films that show ligamentous laxity have seen that ligamentous laxity is revealed on certain motions and not others.
The reason is simple. Even with DMX, the viewer cannot see the ligaments. The structural integrity of the ligaments can only be assessed by observing the movement of the vertebrae in relationship to other vertebrae. Only by using X-rays taken during movement can the accurate and complete assessment of ligamentous integrity be done. It is only abnormal movement of the vertebrae that reveals the ligamentous laxity caused by the excessive stretching of the spinal ligaments. Conversely, when the cervical spine is not moving, there is no way to assess the relative motion of the vertebrae in relation to each other.
For 20 years, the AMA Guides have recognized “Alteration of Motion Segment Integrity” (AOMSI) as the basis of permanent impairment of the spine and have recognized that they cannot be determined by physical examination. Instead, flexion-extension X-rays are required:
Motion of the individual spine segments cannot be determined by physical examination, but is evaluated with flexion and extension roentgenograms (see Figures 15-3a through 15-3c) AMA Guides, (5th Ed. 2001)
But how can static X-rays show abnormality occurring in motion? It is simply nonsense to suggest that that could happen. Instead, motion X rays are needed to show motion abnormalities!!!
Note: During the acute phase of the injury, muscle spasm creates hypomobility of the cervical spine. Accordingly, the abnormal excessive motion resulting from ligament damage cannot be expected to be revealed on digital motion X-ray.
How does DMX work?
The concept is quite simple. DMX is simply a “moving picture” using a series of X-rays to create a “movie.”
X-rays were discovered in 1895 by Professor Roentgen in Germany.
Thomas Alva Edison obtained the first patent for a moving pictureor “movie” in 1908. (A movie or motion picture is simply a series of still photographs shown on the screen moving from one image to another with such speed that the human brain perceives it as a moving image.)
So why did it take so long to put 2 + 2 together, adding the X-ray and the moving picture together? The problem was that of the excess radiation that previously would result from taking all of the X-rays that are necessary to create an X-ray “movie.” The problem has been solved.
Digital Motion X-ray utilizes X-ray technology, and couples it with new digital and optic technology in the image intensifier to create high-resolution images of the spine and skeletal system in real-time motion. DMX can produce 2700 still X-rays with the same radiation dose as the seven (7) view Cervical Davis series.
DMX testing is performed while the patient is in a weight bearing standing position and moving the body through different arcs of motion. Each arc of motion is specific to test an anatomical structure (Specific Group of Ligaments). Each arc of motion is a complete independent study that focuses on the anatomical structures found in that arc of motion.
The intended use for Digital Motion X-ray is to visualize suspected intersegmental joint dysfunction by evaluating all 22 major cervical ligaments with 2700 X-ray images. DMX is the only moving diagnostic test that is performed in a weight bearing position. (This is not a “chiropractic X-ray” designed to look for “subluxations”).
There are two types of Ligament Injuries:
- Sub-failure-When a ligament stretches or partially tears.
- Complete failure-When a ligament is completely severed.
Digital Motion X-ray is the only test that will detect sub-failure ligament injuries. MRI does not have the resolution to detect the stretching or an elongation of a ligament. MRI can detect a complete failure, which is commonly seen in the knee and shoulder. Sub-failure ligament injuries are most commonly seen in the Cervical Spine, TMJ, and Wrist.
DMX can provide valuable information about the stability of all 22 major ligamentous structures in the cervical spine (anterior and posterior longitudinal, facet/capsular, alar, transverse, and accessory ligaments). The upper 30% of the cervical spine gets its stability from ligaments only. There are NO discs in the upper 30% of the cervical spine between Occipital C1 and C2. Digital Motion X-ray is used in demonstrating posttraumatic instability in the neck that may be responsible for posterior neck pain, headaches, and referred pain.
DMX provides objective proof of injury which provides substantiation to insurance companies for continued treatment.
DMX can detect ligamentous laxity that static X-rays cannot see.
Because DMX can X-ray the vertebrae in motion, it is able to detect ligamentous laxity that static X-rays cannot see. As noted by Foreman/Croft, static X-rays don’t reveal major ligamentous injuries:
Most of these (static X-ray) studies…fail to define movement in a dynamic sense…deviation from the normal biokinetics may occur somewhere between these arcs of motion, which would not be visualized by static radiographic techniques.
Foreman/Croft reference a study by Buonocore in which 68% of the whiplash injuries studied by DMX were interpreted as abnormal. Another study by Woesner and Mitts reported that DMX detected abnormalities in 35% of the plain film studies that were interpreted as normal.
DMX is respected by the chiropractic community.
In 1995, Foreman/Croft stated that:
Videofluoroscopy is important in the evaluation of ligamentous instability… several studies have indicated the value of videofluoroscopy in the evaluation of certain types of soft tissue lesions of the neck… clinicians trained in the interpretation of these studies are able to interpret them reliably (p. 53).
They continue to state that:
(Videofluoroscopy has an) important role in the diagnosis of instability of the cervical spine and, to some extent, in determining the prognosis regarding future disability. For example, making them has shown that the healing of a ligamentous structure is generally incomplete; this instability may result in early and accelerated degenerative changes (Citing studies done by Panjabi and others).
DMX has been approved by the Council on Chiropractic Practice: Vertebral Subluxation in Chiropractic Practice Guidelines, 3rd Ed, Council on Chiropractic Practice, 2008, p 318:
Videofluoroscopy may be employed to provide motion views of the spine when abnormal patterns are clinically suspected. Videofluoroscopy may be valuable in detecting and characterizing spinal kinesiopathy associated with vertebral subluxation.
DMX is respected by the U.S Government.
The AHQR (Agency for Healthcare Research & Quality of the U.S. Department of Health & Human Services) recommends DMX in two separate practice guidelines. The Guideline: Vertebral Subluxation in Chiropractic Practice states:
Videofluoroscopy may be employed to provide motion views of the spine when abnormal motion patterns are clinically suspected. Videofluoroscopy may be valuable in detecting and characterizing spinal kinesiopathology associated with vertebral subluxation.
The Guideline: Management of Whiplash Associated Disorders states:
Videofluoroscopy screening may be useful in and for evaluating for cervical instability injuries. Motion MRI (kinetic MRI) has been shown to demonstrate significant differences in biomechanical function between normal patients and injured patients following rear-end, low-impact motor vehicle collisions.
DMX is approved by the FDA. The FDA has classified the dynamic motion X-ray system with a device classification name of “image-intensified fluoroscopic X-ray system”, a regulation number of “892.1650”, assigned a 510(k) number of “k943272”. The machine has been classified as a “class ii” device. Section 892.1650. Image-intensified fluoroscopic X-ray system, and is a device intended to visualize anatomical structures by converting a pattern of x-radiation into a visible image through electronic amplification. This generic type of device may include signal analysis and display equipment, patient and equipment supports, component parts and accessories.
The Centers for Medicare and Medicaid Services further support the appropriateness of fluoroscopy as an examination technique utilized to determine biomechanical abnormalities (subluxation). (Source: Medicare Coverage Database; LCD for Chiropractic Service (manual spinal manipulations) (l15759).
DMX is respected by the medical community.
Digital motion X-ray is well accepted and acknowledged in the medical community as well.
The American Academy of Pain Management’s Practical Guide to Clinicians, 5th Edition states:
…digital motion radiography is currently a valuable diagnostic method in evaluating painful hyper-mobility and instability of capsular and axial ligaments in the cervical spine.
The American College of Occupational Medicine’s Practice Guidelines, 2d Ed. 2004 (American College of Occupational and Environmental Medicine) states:
If probable ligamentous injury with persistent, pain, consider fluoroscopically directed flexion study.
Respected medical doctors (MDs) have publicly proclaimed DMX to be a valuable diagnostic tool. John H. Bland, M.D., Professor of Medicine, University of Vermont, in his book entitled Disorders of the Cervical Spine (1987), said:
Video fluoroscopy is the most valuable technique in analyzing cervical spine motion. The stability of the cervical spine depends on bony structures only to a minor degree; stability depends to a major degree on the ligamentous structures.
Such injury is not always detected on static plain film X-rays (standard roentgenograms). The next best medically reasonable diagnostic tool for determining ligamentous injury (a biomechanical source of pain) is the fluoroscopic exam.
Robert Baily: Professor of Orthopedic Surgery, University of Michigan in The Cervical Spine (1974), chapter 3, Dynamic Anatomy and Cineradiography of The Cervical Spine said this:
Video fluoroscopy shows abnormal secondary to soft tissue (ligamentous) damage. Stability is dependent on ligaments.
Ruth Jackson, M.D., Instructor of Orthopedic Surgery at Baylor University, in her book entitled The Cervical Syndrome (1977) said:
Video fluoroscopy shows areas of limited or unstable motion resulting from ligamentous and capsular injuries.
DMX has been accepted as reliable evidence by the courts.
It seems foolish to even suggest that there might be any question as to whether the courts would accept a DMX as reliable evidence. It has now been 118 years since Dr. Wrench had discovered X-rays as a technology
that could be useful in the detection and diagnosis of various physical conditions. In 1908, Thomas Alva Edison obtained the first patent for a “moving picture” which simply moves a series of still photographs past the human eye with such speed that it appears to be “moving.” DMX simply combines technology that has been respected for more than 100 years.
Accordingly, the courts have acknowledged DMX as reliable evidence. In Graftenreed v. Seabaugh, 268 s.w.3d 905 (Ark. Ct. App. 2007) the Arkansas Court of Appeals made these statements:
Generally, a chiropractor is qualified to testify in a personal injury action concerning matters within the scope of the profession or practice, and may testify as to the permanency of an injury, as well as its probable cause. DMX evidence is reliable, and is accepted by the chiropractic and medical communities. Appellant argues that DMX technology does not meet the Daubert standard because it has not been proven to aid in diagnosing or treating any injury and that DMX gives no more information than standard X-rays. Appellant also asserts that the scientific community has not generally accepted the use of DMX is for diagnosing or treating any injury or ailment. We disagree. Here, there is no question that this evidence was prejudicial to Appellant’s position, however, we cannot say that it was unfairly prejudicial. Appellant next argues that the trial court erred in admitting the DMX evidence because there was no proof as to which accident caused the ligament damage referred to in the radiologist report. According to Appellant, even if the DMX has indicated injury, there was no proof that it was caused by the January 2001 accident. * * * there is more than sufficient evidence to let the jury decide whether Ms. Woods’ injuries were caused by the 2001 accident. Appellees presented testimony that her symptoms began immediately after the wreck; that they continued over several years; that the 2003 accident did not exacerbate them; and that the pain and problems she was experiencing at the time of trial were the same as those that began right after the 2001 wreck.
Other cases that support the admissibility of fluoroscopy. See Hughes v. Denny’s Restaurant, 328 so.2d 830 (Fla. Supreme Court 1976); Destin v. Sears, Roebuck & Co., 803 s.w.2d 113 (Mo. Dist. Ct. App. 1990); Cognata, et.al. v. Weishaupt, et.al., bc243305 (Ca. Los Angeles County Superior Court 2002).
CRMA can quantitatively analyze the extent of the ligamentous laxity.
CRMA is Computerized Radiographic Mensuration Analysis, or CRMA. It is also called “digitized X-ray.” The term “mensuration” simply means “the measurement of geometric quantities.” Medical and chiropractic doctors have, for nearly 100 years, been measuring the translational and angular malpositioning of vertebrae.
CRMA means to measure radiographics (X-ray) using a computer. Thus CRMA provides for accurate, computerized measurement of the malpositioning of vertebrae due to ligamentous laxity.
CRMA is a valuable tool to chiropractic and medical practitioners. It assists in arriving at a differential diagnosis and establishing an appropriate treatment plan.
For patients, it provides substantiation for pain that might otherwise be labeled as “secondary gain,” “somataform disorder,” or just the old fashioned terms of “faking” or “malingering.”
For lawyers and their clients, it is a “blockbuster” development. It provides objective proof of ligamentous injury that has been the major cause of chronic pain and disability in CAD injuries.
CRMA can be used to establish a percentage impairment rating using the AMA Guides rating system.
For 20 years, the AMA Guides have recognized “Alteration of Motion Segment Integrity” (AOMSI) as the basis of permanent impairment of the spine and have recognized cannot be determined by physical examination. Instead, flexion-extension X-rays are required:
Motion of the individual spine segments cannot be determined by physical examination, but is evaluated with flexion and extension roentgenograms (see Figures 15-3a through 15-3c) AMA Guides, (5th Ed. 2001), pg. 379.
But how can static X-rays show abnormality occurring in motion? It is simply nonsense to suggest that that could happen. Instead, motion X rays are needed to show motion abnormalities!!!
DMX scans can be used to provide an AMA based disability rating.
The AMA Guides to the Evaluation of Permanent Impairment, 5th Ed. (2000), p. 392, states that Alteration of Motion Segment Integrity (AOMSI) results in a 25-28% impairment rating in each of the following cases:
Alteration of Motion Segment Integrity or bilateral or multilevel radiculopathy; alteration of motion segment integrity is defined from flexion and extension radiographs as at least 3.5 mm of translation or one vertebrae on another, or angular motion of more than 11 degrees greater than at each adjacent level.
But what about translation at lesser levels? What about angular irregularity less than 11 degrees? Assessments of impairment levels less than that specified in the AMA Guides is appropriate. As stated in Foreman/Croft:
To adopt 3.5 mm of translation as the minimal criterion for anterior subluxation is to leave the majority of mild to moderate instability unclassified.
Translations greater than 2.0 mm have been determined toindicate ligamentous disruption. See Looby,”Spine Trauma,” Radiologic Clinic of North America, Vol 49, No 1, pp. 129-163 (2011).
In another study, measurement of 1 mm translation and/or 7 degrees of angular variation has been considered to be clinically significant and indicative of abnormal flexibility of the cervical spine. See Spine, Vol 3:256-261 (2001).
It, therefore, makes perfect sense that translations less than 3.5 mm. should result in impairment ratings as follows:
3.5 = 25
3.0 = 20
2.5 = 15
2.0 = 10
1.5 = 5
And angular irregularity should result in impairment ratings as follows:
11 degrees = 25
10 = 20
9 = 15
8 = 10
7 = 5
It is true that the AMA Guides does not recognize these numbers, affirmatively or negatively. However, the above numbers are a totally logical conclusion based on the literature.
How do we know that the ligamentous laxity was caused by CAD trauma?
The causal connection between the trauma and the ligamentous laxity is probable for each of the following reasons:
- If the patient was asymptomatic before and immediately acutely symptomatic after the trauma, the causal connection should be clear.
- Motion segment alteration is extremely rare in the absenceof trauma. The AMA Guides states:
When routine X-rays are normal and severe trauma is absent, motion segment alteration is rare; thus, flexion and extension X-rays are indicated only when the physician suspects motion segment alteration from history are findings on routine X-rays.
AMA Guides, 5Ed. 2001, pg. 379.
- If the DMX shows ligamentous laxity that is present at specific levels and not generally throughout the spine, it is highly probable that the laxity is traumatic rather than the result of natural. As stated in Lin, “characteristics of sagittal vertebral alignment in flexion determined by dynamic radiographs of the cervical spine,” Spine, Volume 26(3), pg. 256 – 261.
The aging changes of the cervical spine should be similar at each level, if no trauma affects a specific level.
Lin cites numerous articles supporting this concept.
- If the ligamentous laxity occurs in whole or in part in the upper cervical spine, that is an additional indicator that the laxity is trauma-induced because laxity due to non-traumatic degeneration typically occurs at the lower cervical levels rather than the upper levels. See Dvorak, et.al. Clinical validation of functional flexion/extension radiographs of the cervical spine. See also Spine, 18(1), pp. 120-7(1976).
- If the ligamentous laxity is centered at the C4-5 joint, it is likely due to trauma. It is well recognized thatthe C4-5 joint is the single most vulnerable of the cervical spine joints and the location at which ligamentous laxity is most likely to occur. Accordingly, if the ligamentous laxity includes that joint, it is an additional indicator that the laxity was caused by traumatic forces.
Ligamentous Laxity Causes Accelerated Degeneration of the Intervertebral Discs.
The concept is quite simple. Biomechanical studies have established the following principles:
-Ligaments of the primary source of stability and human spine.
-Ligaments, and intervertebral discs work together, in tandem, to provide stability to the spine.
-Loss of ligamentous support, ligamentous laxity, places increased stress on the intervertebral discs, resulting in accelerated degeneration of the intervertebral disc.
Foreman/Croft reports that injuries to the anterior longitudinal ligament and intervertebral discs typically produce immediate symptoms, whereas delayed instability is not uncommon in injury to the other spinal ligaments of the cervical spine. (359) They report that “ligaments heal with scar tissue, which is less elastic, less resilient, less pliable, and less resistant to shear and tensile forces than the original tissue” adversely affecting mobility and extensibility and causing altered biomechanics of the spine. They note that “the lack of motion at one level will be compensated for by hypermobility at adjacent levels, which in turn usually will result in degenerative disc disease and osteoarthritis sometime in the future.”
Foreman and Croft cite studies by the eminent Dr. Ruth Jackson and Ehni who explain the biomedical aspects of the process of accelerated degeneration as follows:
Acute injury (sprain) of the joint produces synovial effusion, histamine release, capsular ligament is stretched or tore, bleeding, and associated clinical disabilities. Some of this is visible and palpable in joints in the extremities, such as the ankle and knee, but not in those of the spine. With repetition of the traumatic process and with chronic stress and the joint from sharing and other forces, as the disc fans and the superior facet moves cephalad under the inferior facet of the vertebra above, a chronic synovial reaction becomes established, which extends to the underlying articular cartilage. The cartilage undergoes fibrillar change, softens and becomes rough and eroded. Stresses in the capsule and periosteum result in marginal osteophytosis, which may encroach on the underlying nerve root. A loose body may develop in the joint cavity, or an austere olefinic process may fracture of life rear loosely attached in or near the foramina. The facetal bone may thicken or hypertrophy, and the laminae may do so as well, but not to the same degree as seen in the lumbar spine. Degenerative enlargement of facets with irritative compression of one or more cervical roots may occur…
They note that the zygapophyseal joint is particularly susceptible to this accelerated degeneration process.
Numerous medical journals have established that whiplash injury causes changes that predispose the victim to “premature degenerative disc disease.” See The Neurology of Trauma 1992; 10(4):975-997; Injury 1993; 24:549-550. See also Journal of Bone Joint Surgery 1974; 56A:1675- 1682(reporting a study that found that 39% of whiplash victims had accelerated degeneration at 5 years post-injury).
The concept is quite simple. Biomedical studies have established the following principles:
-ligaments are the primary source of stability in the human spine.
-ligaments and intervertebral discs work together, in tandem, to provide stability to the spine.
-loss of ligamentous support, ligamentous laxity, places increased stress on the intervertebral discs, resulting in accelerated degeneration of the discs.
Delayed instability of the spine due to ligamentous laxity is recognized in the medical literature. DMX is a valuable tool in detecting delayed instability of the ligaments. See Cusic, Clinical Biomechanics, Vol. 17, No 1, pp. 1-20 (2002)
When ligamentous laxity is demonstrated, repeat MRIs can, in some cases, objectively prove accelerated degeneration.
We have known for many years that CAD injury predisposes the victims to accelerated degeneration. Previously, that concept has only been a hypothetical one as it relates to any given patient/client. Recently, however, the lawyers at the Schmidt Law Firm have discovered that, in some cases, there is objective, irrefutable proof of highly accelerated degeneration in some of the clients who have been found on DMX to have significant ligamentous laxity. One of those cases is presented below. In “Gina’s Case,” a 14 year old, previously healthy girl was found to have the equivalent of 30 years of accelerated degeneration that had occurred in only 2 years!!!
The combination of DMX, CRMA, and Motion MRI can be extremely valuable in proving major impairment in cases that previously were dismissed as minor “soft tissue” injuries.
DMX provides objective proof of the existence of both translational laxity and angular laxity in ligaments.
CRMA provides a scientifically reliable method of accurately measuring or quantifying the exact amount of laxity in each category.
Weight-Bearing Flexion/Extension MRI provides a method of proving the existence of accelerated degeneration.
Together, they form the “Golden Pyramid” of Objective Proof of ligamentous injury.
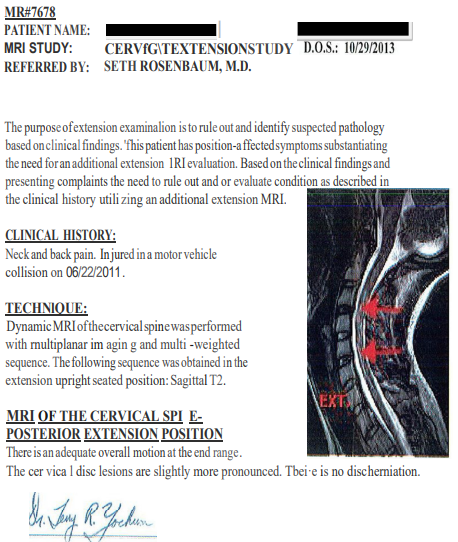
Motion MRIs provide a method of detecting herniations that are not observable in conventional MRIs.
SUMA MRI has developed a new technology that may be as revolutionary as Digital Motion X-rays, namely “Motion MRIs.” This procedure involves taking MRIs in a number of positions, or stations, throughout the flexion extension cycle. Remarkably, it has been shown that some herniations will be revealed at one station but not others. Some will be revealed at one station, then disappear at other stations, and reappear at yet others.
The bottom line is that Motion MRIs can reveal herniations that would not be detected by other forms of MRIs.
DMX provides proof of the cause of Facet Joint Injuries.
Recently, authoritative and reliable medical research has established that the primary cause of chronic pain in the victims of CAD trauma is injury to the facet joint. Reliable biomedical research has established that facet joint pain is primarily due to injury to the capsular ligament and to some extent of the anterior longitudinal ligament. Research is also established that injury to the synovial fold may be a secondary cause. See Yogandando et al., Biomechanics of the Cervical Spine, Journal of Biomechanics (2001).
The internal facet joint injury provokes pain in the medial branch nerve. Radiofrequency neurotomy (RFN) provides relief of pain in the medial branch nerve by coagulating the nerve so that it no longer transmits the pain message to the brain. However, RFN procedures do absolutely nothing to cure the underlying injury in the facet joint.
Now, as Paul Harvey would say, the other side of the story: DMX now provides a method of proving damage to the capsular ligament and the anterior longitudinal ligament!!!
Ligamentous laxity is the primary cause of Myofascial Pain Syndrome and trigger points.
Chronic muscular symptoms of myofascial pain syndrome with trigger points are the result of the muscle overload resulting from the muscles working excessively to compensate for ligamentous laxity. Foreman/Croft states that muscles heal within “a few weeks” leaving “myofascial pain disorders” in which the muscles serve as the “end organs” of the “long term manifestations…of late whiplash” (p. 15, 384).
Case studies-“Gina’s Case” and “Bruce’s Case” provide objective proof of accelerated degeneration of intervertebral discssecondary to ligament damage.
It has been recognized for decades that whiplash trauma and injurycauses long-term accelerated degeneration of the spine. However, that concept has been largely theoretical—until now. In several cases, the Schmidt Law Firm has “doubled back” and sent clients for repeat MRIs of the cervical spine. The results have been amazing! Two such cases are presented here.
Gina’s Case
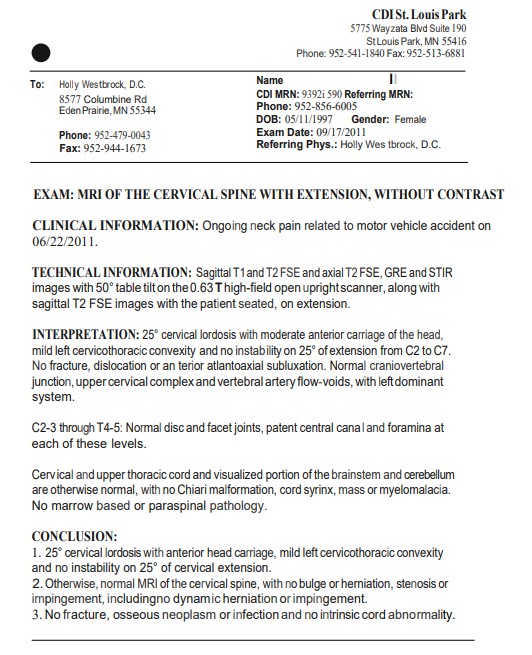
Gina was injured in a car crash as a 14 year old. Her MRI, done shortly after that collision, was totally normal. Two years later, and $32,000 of chiropractic and medical treatment, as well as physical therapy and massage therapy, and she was still symptomatic. However, DMX showed significant ligamentous laxity.
CRMA showed translational instability of 3.5 mm, sufficient to establish an AMA rating of 25%. It also showed angular instability of 12.5%, also sufficient to establish another AMA rating of 25%.
Repeat MRIs then showed significant desiccation and bulging of her intervertebral discs—proof of accelerated degeneration.
This evidence formed the basis of a claim that Gina’s cervical spine, in a 14 year old that was totally healthy before her car accident, had “aged” the equivalent of 30 years in the course of only 2 years!!! Her medical doctor then reported the following:
It should be noted that MRIs of Gina’s cervical spine which were performed on September 17, 2011, were unremarkable with the exception of the 25 degree cervical lordosis that was noted. The finding of cervical lordosis indicates that the ligamentous laxity which is noted on the recent DMX studies was present at that time. That ligamentous damage would not be expected to show on static MRIs. However, it is apparent that Gina has, in the intervening 2 years experienced significant degeneration of her cervical spine which is an expected result of the ligamentous damage.
It is well established in the medical literature that the ligaments of the spine and the intervertebral discs work in tandem to provide stability to the spine. When the ligamentous are stretched and damaged creating ligamentous instability, excessive stresses are imposed on the intervertebral discs which cause accelerated degeneration of the discs. These studies provide objective evidence that Gina’s ligamentous instability has resulted in significantly accelerated degeneration, as evidenced by the disc desiccation and bulging.
It should also be noted that these studies provide objective evidence to support my diagnosis of myofascial pain syndrome. Myofascial pain syndrome is the result of overload imposed on the skeletal muscles in the neck and back as a result of the ligamentous laxity. Simply put, myofascial trigger points result from the fact that the muscles are working overtime to compensate for the ligamentous laxity.
The result was objective proof of disc desiccation and bulging discs which occurred over a 2 year period. Simply put, Gina’s ligamentous injury had produced laxity which imposed abnormal stresses on the intervertebral discs, causing grossly abnormal degeneration. In the course of only 2 years since her whiplash injury, Gina’s neck had “aged” or “degenerated” the equivalent of 30-40 years!
For more detail regarding Gina’s case, see Exhibit A.
Bruce’s Case
Bruce’s case is even more dramatic. Bruce was injured in a car accident when he was 45 years old. His MRI showed some generalized degeneration, mostly mild desiccation and some facet arthrosis which would be typical and expected for a 45 year old with a history of doing physical labor while working as a carpenter/fix-it-man, but nothing significant. 4 years later, a DMX showed major ligamentous laxity-much more than would occur naturally, especially when considering that he totally stopped doing any significant physical work after his accident.
Again, repeat MRIs showed dramatic accelerated degeneration with 3 large herniations and impingement on the nerve roots at all 3 levels:
MRI of the Cervical Spine dated 12/17/13 (SUMA) with the following elements:
(1) Left paracentral posterior disc herniation (4mm) at C3/4;
(2) Broad-based posterior disc herniation at C5/6(6mm) and C6/7 (4mm);
(3) Annular bulge at C2/3 and C4/5;
(4) Dehydration of the discs as noted above;
(5) Mild loss of disc height;
(6) Straightening of the normal lordosis;
(7) Moderate stenosis of the bilateral intervertebral neural foramina at C5/6 and C6/7 with impingement of the bilateralC6 and C7 nerve roots;
(8) Moderate stenosis of the left intervertebral neural foramen at C3/4 with impingement of the left C4 nerve roots; and
(9) Mild central canal stenosis at C3/4, C5/6 and C6/7.
Based on this new MRI, his medical doctor concluded that he had experienced the equivalent of 30 years of degeneration since his motor vehicle collision:
It is well established in the medical and biomedical literature that injuries of the type that Mr. Bruce experienced in the November 18, 2008, motor vehicle accident produced ligamentous deformation which is plastic in nature so that it does not return to its prior condition, thus producing instability of the cervical spine as now documented on Mr. Bruce’s DMX studies. Further, the ligamentous instability then results in placing stresses on the intervertebral discs, thus producing advanced changes that are quite dramatic and have occurred in just 3 years. In this case, Mr. Bruce’s degeneration cannot be explained by normal aging process. On contrary, this degeneration is the equivalent of 30 years of degeneration due to normal aging.
The most important aspect of facet joint injury is being overlooked, namely the underlying ligamentous injury.
Recently, trial lawyers have come to realize that facet joint injuries are perhaps the most important aspect of spinal injuries. Medical research has established that facet joint injury is the primary cause of 60% of the cases of chronic pain lasting more than one year post injury.
Radiofrequency Neurotomy (RFN) has become increasingly recognized as a form of treatment that can provide major relief to the victims of facet joint pain.
The medial branch nerve transmits the pain signals from the facet joint to the brain. RFN, also referenced as radiofrequency ablation or rhizotomy, involves coagulating the medial branch nerve which, in turn, blocks the pain transmission from the facet joint and provides relief from the facet joint pain.
RFNs have been determined to be successful in 90% of the cases where the patients are properly pre-selected. However, the beneficial effects of RFN only last somewhere between 8-15 months—and then the pain returns. That is true because the RFN does nothing to heal, cure or improve the injury to the facet joint.
The RFN procedure can then be repeated indefinitely. Studies show that the repeat procedure will be successful more than 90% of the time in cases where the first RFN was successful.
Personal injury cases involving RFN treatment have been successful in producing some rather large jury verdicts for several reasons:
(1) RFN procedures, including the test injections, cost approximately $10,000-$12,000. If they need to be repeated, the projected cost of future medical expenses will be well in the six figure range, thus significantly increasing the potential size of the jury verdict. (Note: If a 35 year old will need RFNs for life, and has a life expectancy of 44.6 years, then the future projected medical expenses would be $490,600.00); and
(2) The fact of successful treatment with RFN provides strong evidence of the existence of the facet joint injury. (If the pain goes away with treatment of the facet joint, that proves that the facet joint was the cause of the pain.)
In most cases, the fact that RFNs do absolutely nothing to heal or cure the underlying injury is completely overlooked. In many cases, the lawyers produce absolutely no evidence to establish the nature and extent of the underlying injury.
The answer can be found in the biomedical research. The primary cause of facet joint injury is damage to the capsular ligament. See Yoganandan, “Biomechanical analyses of whiplash injuries using an experimental model,” Accident Analysis and Prevention, Vol 34, No 5, pp. 663-671 (2002).
Here, the missing link often is supplied by the DMX. In those cases where the DMX shows damage to the capsular ligament, objective proof exists to confirm the existence of the capsular ligament injury and, thus, the underlying injury which has been causing the pain in the medial branch nerve. Because the ligamentous laxity that causes the facet joint pain also causes accelerated degeneration of the spine, patients who are candidates for RFN treatment can be expected to get worse over time because of this accelerated degeneration.
Then, when subsequent MRI scans provide evidence of the accelerated degeneration which results from the existence of the ligamentous laxity which, in turn, places more stress and stain on the intervertebral disc structure, the full consequences of the injury are brought to light.
Respectfully submitted,
Douglas E. Schmidt
Schmidt Law Firm
Appendix A-GINA’S CASE-
A CLASSIC EXAMPLE OF HOW DMX & MULTIPLE POSITION MRI CAN ESTABLISH PERMANENT LIGAMENTOUS DAMAGE
- Serious ligamentous injuries have been dismissed as “soft tissue sprain/strain” injuries of minimal consequence because of the lack of objective proof.
- We now have that proof of the ligamentous damage!!! DMX provides that objective proof.
- We also now have objective proof of accelerated degeneration resulting from ligamentous laxity!!!
Gina’s Case is a classic example.
BEFORE DMX:
- Gina was a 14 year old girl who sustained a whiplash injury.
- After 2 years of treatment, by DC, MD, PT and Massage ($32,000.00), she continues to experience major pain and disability.
- The MRI was “unremarkable” in all aspects. -The Chiropractic diagnosis was “sprain/strain.”
- The MD diagnosis was “ligamentous injury” with no objective proof.
- The offer of settlement was only $2,000.00 more than the medical bills.
THE DMX STUDY PROVIDED
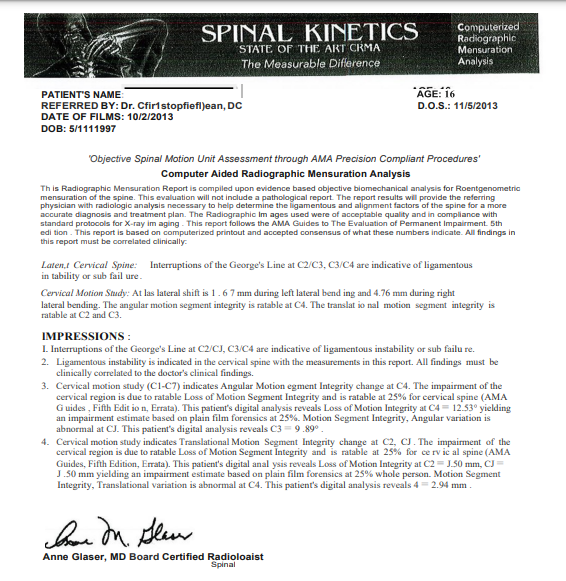
SUBSEQUENT MRI SCANS PROVIDED OBJECTIVE PROOF OF ACCELERATED DEGENERATION DUE TO LIGAMENTOUS LAXITY:
-Multi-positional MRIs at SUMA show accelerated degeneration, i.e. multiple disc bulges and disc desiccation.
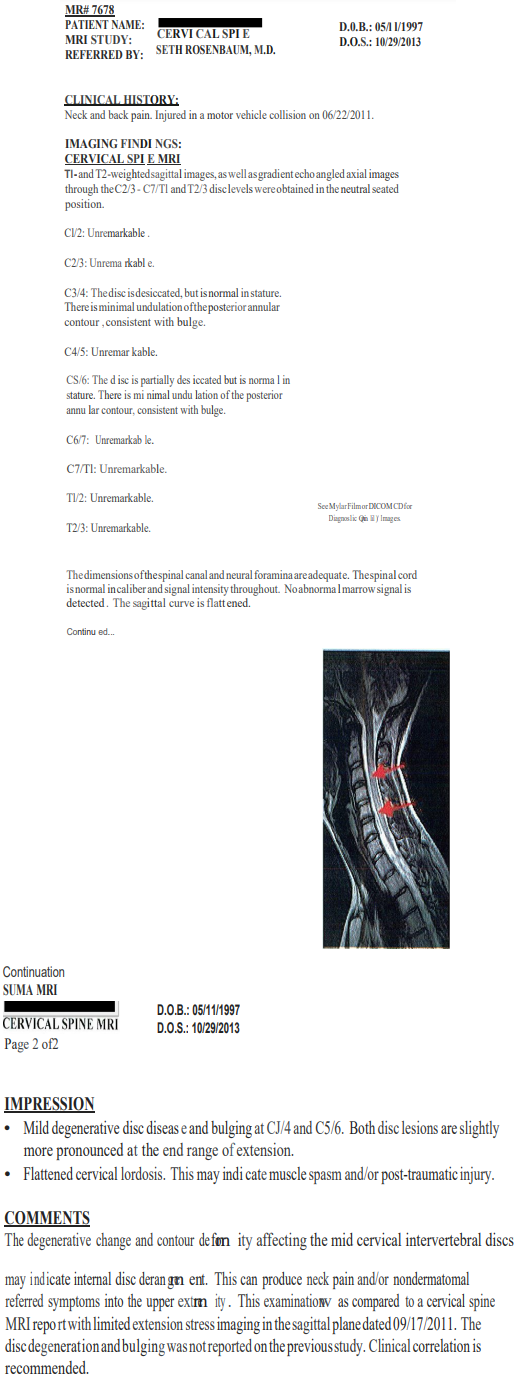

BOTTOM LINE-MAJOR ACCELERATED DEGENERATION:
- Ligamentous injury to a 14 year old girl, previously healthy, has resulted in two impairments of her cervical spine, each rateable pursuant to AMA Guides at 25% of the whole body.
- Proof of accelerated degeneration of her spine.
- Her spine has aged the equivalent of 30-40 years in 2 years!!!
Appendix B- Bruce’s Case
Bruce’s case is even more dramatic than Gina’s in objectively proving accelerated degeneration secondary to ligamentous injury.
Bruce was injured in a car accident when he was 45 years old. His MRI showed some generalized degeneration, mostly mild desiccation and some facet arthrosis which would be typical and expected for a 45 year old with a history of doing physical labor while working as a carpenter/fix-it-man, but nothing significant.
4 years later, a DMX showed major ligamentous laxity-much more than would occur naturally, especially when considering that he totally stopped doing any significant physical work after his accident.
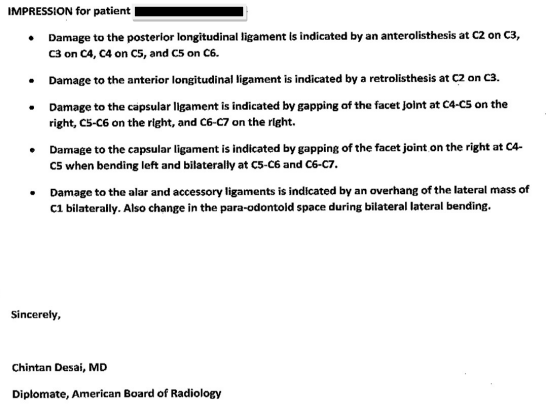
IMPRESSION for patient BRUCE:
- Damage to the posterior longitudinal ligament is indicated byan anterolisthesis at C3 on C4.
- Damage to the capsular ligament is indicated by intervertebralforaminal encroachment of the facet joint at C3-C4 bilaterally.
- Damage to the alar and accessory ligaments is indicated by an overhang ofthe lateral mass of C1 to the left.
Again, repeat MRIs showed dramatic accelerated degeneration with 3 large herniations and impingement on the nerve roots at all 3 levels: MRI of the Cervical Spine dated 12/17/13 (SUMA) with the following elements:
(1) Left paracentral posterior disc herniation (4mm) at C3-4;
(2) Broad-based posterior disc herniation at C5-6 (6mm) and C6-7 (4mm);
(3) Annular bulge at C2-3 and C4-5;
(4) Dehydration of the discs as noted above;
(5) Mild loss of disc height;
(6) Straightening of the normal lordosis;
(7) Moderate stenosis of the bilateral intervertebral neural foramina at C5/6 and C6/7 with impingement of the bilateralC6 and C7 nerve roots;
(8) Moderate stenosis of the left intervertebral neural foramen at C3/4 with impingement of the left C4 nerve roots; and
(9) Mild central canal stenosis at C3/4, C5/6 and C6/7.
Continuation

Appendix C-Tony’s Case
In the first case in the upper Midwest in which DMX was offered into evidence, the result was amazing.
The case was LUCI V. PARROT which was tried to a jury in St. Croix County, Wisconsin. (Hudson, Wisconsin is the county seat.)
The last offer before trial was $10,000.00.
The jury verdict at end of trial was $743,188.95 DMX video was played to the jury,
Their eyes were “bugged;”
They were leaning forward in their seats to look; and
They asked to see it replayed!
Doug Schmidt says,
“It was the most powerful and persuasive single piece of evidence that I have ever seen in a courtroom in over 40 years of trial experience.”